Article originally published 17th August 2022, updated 11th June 2024.
Introduction
Artificial intelligence
In the last year, hearing about artificial intelligence (AI) has become unavoidable as both significant leaps forward have been made in the technology and tools have been made available allowing the general public to try out AI. Within healthcare, the expansion of new technologies such as AI has opened up novel ways to manage and diagnose diseases. Given this, Remap Consulting is revisiting AI and what it means for healthcare. In this article, we shall look back over AI in diabetes, highlighting recent updates.
Diabetes
Around the world, it is estimated that 422 million people have diabetes, that’s almost 20% of the global population1. Diabetes is a chronic condition where a patient’s blood glucose level is too high. This happens if your body doesn’t produce enough insulin or the insulin that it produces isn’t effective. For all type 1 diabetics and around an 8th of type 2 diabetics2 the treatment is self-monitoring of blood glucose through ‘finger-prick’ blood tests and self-administering the required dose of insulin to try to keep blood glucose levels within range. This means patients are having to make many treatment decisions on the insulin dose frequency and amount. Miscalculations occur frequently which can lead to hypoglycaemic events if too much insulin is administered, this can be dangerous and lead to hospitalisation. Furthermore, regular poor blood sugar control can lead to several long-term complications including nerve damage, kidney damage and sight loss, among others3.
Artificial intelligence in diabetes
AI advances are promising to revolutionise diabetes care by collecting real-time data to aid both the diagnosis and treatment. On a simple level, AI can be described as “leveraging computers and machines to mimic the problem-solving and decision-making capabilities of the human mind”4. This is a particular asset to the management of diabetes, given the complexity of the disease, the need for day-to-day self-management, and the need for continual self-monitoring. Based on the literature that is being published around AI in diabetes, eight areas have been identified where AI could revolutionise the diabetes landscape5:
- Diabetes management and treatment: AI personalises diabetes treatment and insulin dosing
- Public health interventions: Tools developed by AI for assessing and preventing diabetes complications
- Diagnostic and Imaging: To improve medical imaging in diabetes-related areas
- Lifestyle and dietary management (including diabetes prevention): The creation of dietary and lifestyle advice which is quickly and easily customisable to the patient
- Health monitoring: Enhances real-time glucose monitoring and alerts
- Enhance clinical decision-making: Informs and refines medical decisions
- Creation of predictive models: Helps with the forecasting of diabetes progression and patients’ treatment response
- Patient engagement: Boosting patient involvement in their own care through AI-driven tools
All of these options are made possible as AI, in a very short time, is able to analyse and interpret large data sets to predict risks, customise treatments, interpret results to give accurate advice and so on. Incorporating AI into healthcare, and especially into diabetes management, may have the power to reduce the disease burden for affected patients as a more proactive and personal approach becomes possible.
The challenges of securing funding for AI technologies
While many of these initiatives have the power to improve the life of the patient, in many countries, there may still be a substantial challenge in securing funding for an AI-driven tool. Many of these new and developing initiatives may come under the umbrella of digital health apps, which in several markets have a reputation for difficulty coming to market (read our article on how to gain access in the UK here. One reason for this is that the technologies are increasing in complexity at a faster rate than HTA bodies can update their guidance and that many digital health products could go through many updates to improve the technology before any assessment could go from start to finish (read more about how this works in the EU4+UK here. In some countries, notably Germany and Belgium, a solid system exists to access digital therapeutics (DiGA and mHealthBelgium). In other countries such as Spain, guidance on access to digital therapies is very limited, with few examples of success. This could mean that despite some AI-based technologies having the ability to improve patients’ lives, limits in the ability to assess them could mean that they only really have success in the private market.
Hybrid Closed Loop Systems
One AI-based technology that has already been launched in diabetes and continues improving patient care is hybrid closed-loop systems, designed to monitor glucose levels and administer insulin. In this section, we shall discuss hybrid closed-loop systems in more detail.
What are they?
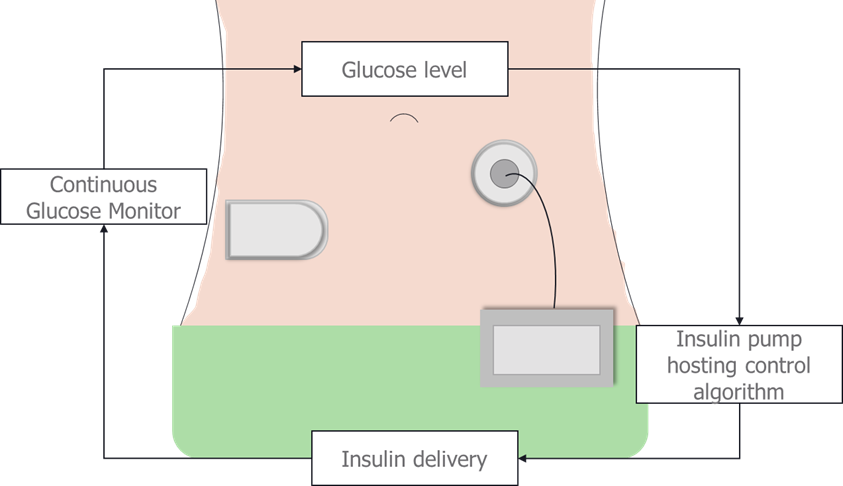
Closed loop systems, also sometimes referred to as an artificial pancreas, monitor blood glucose levels through a CGM. CGMs consist of a tiny sensor under the skin of the abdomen or the arm and are covered with an adhesive patch to hold the transmitter, which sends data from the CGM to a control algorithm, which instructs an insulin pump to administer a specific insulin infusion rate. Insulin pumps are about the size of smart phones and house the algorithm to deliver insulin and the insulin itself. They are attached to a patient with a needle or a cannula which goes under the skin usually on the abdomen and is held in place with an adhesive patch. Thus, the closed loop system removes the need for the patient to monitor their own blood glucose levels and determine the correct dose of insulin. Current closed loop systems are referred to as ‘hybrid’ because patients are still required to calculate bolus insulin before meals as currently available insulins do not act quickly enough to be able to wait for the CGM to detect rising blood glucose levels after a meal. There are several different insulin pumps that have been approved for use in the UK including the mylife Omnipod, Minimed 640G/ 670G, and the Aviva combo amongst others.
What are their benefits?
Prior to the use of hybrid closed loop systems, patient management of their diabetes was very time intensive with diabetics or their carers/parents having to regularly take glucose measurements and make calculations on insulin dose. The hybrid closed loop system has a number of benefits over this7:
- Reduced time spent managing the disease
- Reduced anxiety over ensuring glucose readings have been taken and calculating the insulin dose
- More precise and more frequent insulin dose given, keeping blood sugar more stable
- As blood sugar is more stable hypos are reduced, HbA1c is lowered, and risk of diabetes complications are lessened
How are they funded?
In England, medical devices, such as the components of the hybrid closed loop system, will have to be registered on HealthTech Connect to be considered for a NICE evaluation. If selected the devices will be assessed through the medical technology evaluation program8. However, unlike with technology appraisals a positive recommendation does not lead to a funding mandate and each ICS will decide individually whether to fund the product.
On top of this, the large price tag associated with hybrid closed-loop systems mean they are not available to all comers. In the UK, for example, unless acquiring privately, guidelines states that closed-loop systems are not available for any type 2 diabetics and are only routinely given to type 1 diabetics who are either9:
- Less than 12 years of age
- Have disabling hypoglycaemia when trying to reach their target HbA1c levels.
However, this method of reimbursement where the AI has been bundled with the hardware is more established than if reimbursement was sought for the AI as a standalone digital therapeutic. Unlike some countries such as Germany and Belgium with their DiGA and mHealthBelgium processes, the UK system to reimburse digital therapeutics is still maturing with NICE reforming the process in the near future10.
You can read more about what is required for digital therapeutic reimbursement in the UK and how they are funded in our previous articles.
Will access increase to the wider diabetes community?
The use of AI in regulating blood glucose levels undoubtedly shows promise for both short-term control and long-term outcomes. However, as with all medical technologies, the ability to demonstrate long-term benefits and convince reimbursement authorities that theoretical benefits will play out in practice is difficult. It is, therefore, not surprising that access to the closed-loop system is currently restricted to a narrow group of patients.
The NHS typically focuses on funding and budgets within a two-year timeframe, pushing considerations of long-term cost savings even further from the minds of hospital directors. As diabetes is a chronic disease with complications developing many years after diagnosis, savings from devices such as the hybrid closed loop system are not likely to be seen for a while, despite avoidable diabetes complications costing the NHS £7.7 billion per year10. Until the prices come down for these systems, manufacturers may have to demonstrate better cost savings associated with reduced hypoglycaemic events in the short term, reduced resource usage in well-managed patients and show patients’ improved quality of life with these systems to secure more comprehensive access. Therefore, access to hybrid closed-loop systems isn’t expected to increase in the short term.
Conclusion
The technology driving AI is fast-moving, and though the healthcare sector has been slow to adopt AI to improve patient outcomes, it is becoming more accepted in diabetes. Although, limited changes in the past two years in the diabetes field further highlight the slow movement of AI in healthcare. Though most diabetes devices that use AI currently come with high price tags, which are at least partially responsible for limited patient access, the value of these AI-driven technologies is beginning to be more thoroughly investigated. We can assume that the use of AI in diabetes is the first step in becoming embedded in the treatment pathways for numerous other diseases. As organisations such as NICE update their processes to accommodate the new technology, the hope is that the path to reimbursement will become clearer and pave the way for AI to be adopted in other areas of healthcare. As more people become used to AI in their daily lives, from text and voice recognition to facial recognition to unlock their phones and chatbots, it might be anticipated that patients and healthcare systems also become more comfortable employing AI to help manage their diagnosis, treatment, or administrative processes.
Sources:
- Diabetes. https://www.who.int/health-topics/diabetes#tab=tab_1. Accessed 27 July 2022.
- Basu, Sanjay et al. “Estimation of global insulin use for type 2 diabetes, 2018-30: a microsimulation analysis.” The lancet. Diabetes & endocrinology 7 1 (2019): 25-33
- Complications of Diabetes. https://www.diabetes.org.uk/guide-to-diabetes/complications. Accessed 5th August 2022.
- Artificial Intelligence (AI). https://www.ibm.com/cloud/learn/what-is-artificial-intelligence. Accessed 27th July 2022.
- Khalifa and Albadawy. Artificial intelligence for diabetes: Enhancing prevention disease, diagnosis, and effective management. Computer Methods and Programs in Biomedicine Update. 2024 5:100141
- Hartnell S, Fuchs J, Boughton C, Hovorka R. Closed-loop technology: a practical guide. Practical Diabetes. 2021 Aug;38(4):33-39.
- Closed loop systems (artificial pancreas). https://www.diabetes.org.uk/guide-to-diabetes/diabetes-technology/closed-loop-systems#:~:text=Benefits%20of%20hybrid%20closed%20loop%20systems&text=This%20can%20reduce%20hypos%20and,a%20better%20quality%20of%20life. Acccessed 3rd August 2022
- How we develop medical technologies guidance. https://www.nice.org.uk/about/what-we-do/our-programmes/nice-guidance/medical-technologies-guidance/how-we-develop. Accessed 3rd August 2022.
- Treatment Summary: Type 1 Diabetes. https://bnf.nice.org.uk/treatment-summary/type-1-diabetes.html. Accessed 27th July 2022.
- The Cost of Diabetes Report. https://www.diabetes.org.uk/resources-s3/2017-11/diabetes%20uk%20cost%20of%20diabetes%20report.pdf. Accessed 3rd August 2022.
